Cuff Tear Arthropathy
Michael Fu, MD
As you may recall in our shoulder basics article, the primary function of the rotator cuff is to keep the humeral head (ball) centered on the glenoid (socket) through shoulder motion and activity.
Image courtesy of Visible Body.
This is no small task - there are a number of large muscles (pectoralis, deltoid, latissimus, etc.) exerting hundreds of pounds of force across the shoulder joint as we do push-ups, bench press, swing a tennis racquet, or even just lifting a gallon of milk away from our body.
When the rotator cuff is torn, the shoulder is then unbalanced as the humeral head (ball) no longer remains centered in the glenoid (socket). As the humeral head slides around on the glenoid with shoulder activity, this creates repetitive shear stress at the joint surface, which is poorly-tolerated by the cartilage tissue.
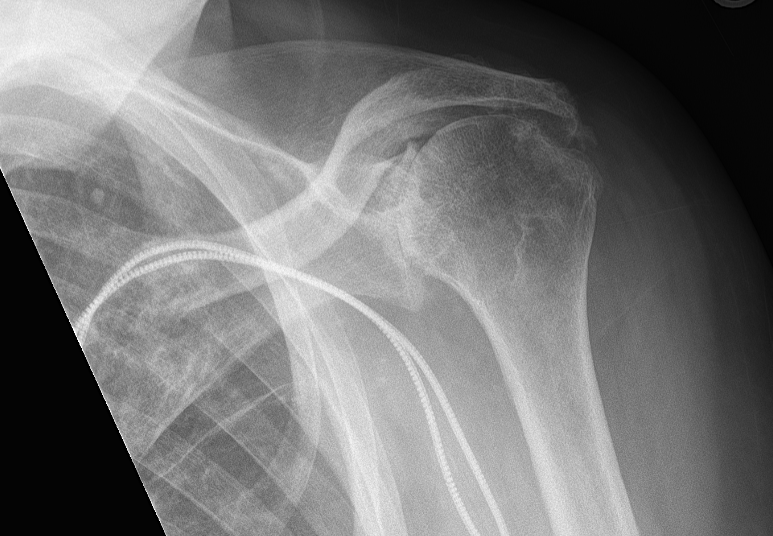
Over a prolonged period of time, a torn or otherwise dysfunctional rotator cuff leads to a specific pattern of shoulder arthritis called Cuff Tear Arthropathy. This is a different condition from primary shoulder arthritis. In cuff tear arthropathy, since the rotator cuff is no longer working to keep the humeral head centered on the glenoid, the humeral head then has a tendency to ride up due to the pull of the deltoid muscle.
Symptoms of cuff tear arthropathy
Similar to patients with shoulder arthritis, those with cuff tear arthropathy most commonly experience pain and stiffness in the shoulder. The location of pain can vary from patient to patient, but most people report feeling a deep-seated pain within the joint. Initially the pain occurs primarily with high-demand activities and certain shoulder positions, but as the disease progresses, pain can occur with more and more activities of daily living. With moderate to severe shoulder arthritis, pain then frequently occurs at night that can interfere with sleep. In fact, night-time pain and poor sleep is the most common reason why patients seek consultations with our office.
Unlike primary shoulder arthritis, however, patients with cuff tear arthropathy often have a profound inability to lift up their arm. This is described as pseudoparalysis or pseudoparesis - “pseudo” because the nerves and muscles that normally lift the arm are still functional, so it is not true paralysis. This occurs because without the rotator cuff centering the humeral head on the glenoid, there is no longer a stable fulcrum to lift up the arm. In severe cases, the humeral head can be so unstable as to “escape” from the glenoid, in a phenomenon called “anterosuperior escape”.
Non-operative treatment
As with other chronic shoulder conditions, we recommend beginning with non-operative treatment. The primary objective is to reduce inflammation, which can be accomplished through activity modification, ice, oral anti-inflammatory medications (NSAIDs, i.e. ibuprofen, naproxen, meloxicam, etc.), oral corticosteroids, corticosteroid (cortisone) injections, and biologic injections such as platelet-rich plasma (PRP). Physical therapy can be helpful in correcting any negative functional or postural adaptations you have made due to shoulder pain. We offer all of these treatments at HSS, and every patient’s response to the various options is different. While none of these treatments actually reverse the progression of arthritis, however, they can provide pain and symptom relief for long periods of time.
Operative treatment
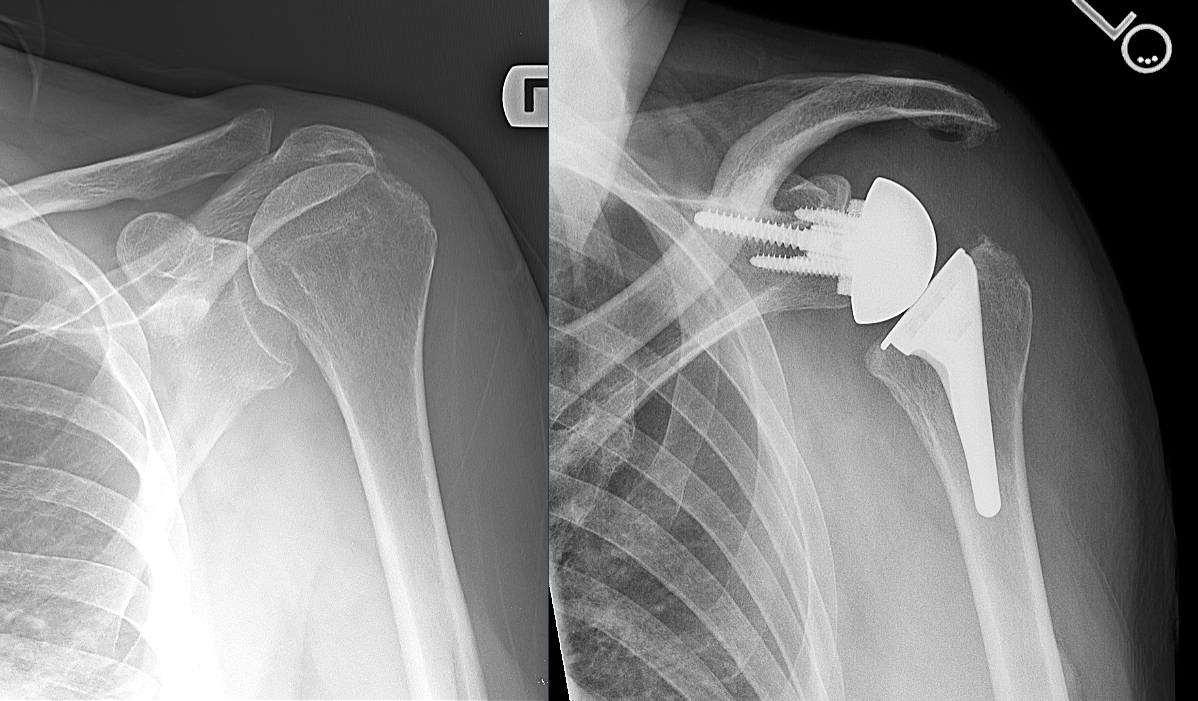
Unlike primary shoulder arthritis, an anatomic total shoulder replacement is not an option for cuff tear arthropathy due to the absence of the rotator cuff. In this case, the definitive treatment for cuff tear arthropathy is a reverse total shoulder replacement. It is called a reverse shoulder replacement because a metal sphere is implanted into the native glenoid (socket), while a socket-type implant is placed where the native humeral head (ball) was.
This reverse total shoulder replacement was pioneered and continually refined by a number of French master shoulder surgeons for decades before it was approved for use in the United States. During my training, I had the privilege of going to France multiple times for courses as well as to specifically spend time with Professor Pascal Boileau in Nice, and Professor Gilles Walch in Lyon.
The reverse shoulder works through several mechanisms. First, there is a higher degree of congruence between the ball and the socket, leading to more intrinsic stability. This helps the implant perform arguably the most important role of the rotator cuff - to keep the shoulder joint centered around a stable fulcrum through shoulder motion. Second, the center of rotation for a reverse shoulder replacement is more medial (towards the middle of the body) relative to the native shoulder joint, which significantly improves the biomechanics of the deltoid muscle, thus allowing it to elevate the arm in the absence of a rotator cuff.
Cuff tear arthropathy before and after reverse total shoulder replacement
Outcomes following reverse total shoulder replacement are generally excellent as well. Due to its unique design, however, it does not recreate the anatomy of your native shoulder. While it is very effective at relieving pain, which is the primary reason for undergoing surgery, reverse total shoulder replacement should not be expected to provide completely normal shoulder function. Every patient is different, and we recommend a personal consultation with our team to review your case and answer any questions you might have.
About the Author
Dr. Michael Fu is an orthopedic surgeon and shoulder specialist at the Hospital for Special Surgery (HSS), the No. 1 hospital for orthopedics as ranked by U.S. News & World Report. Dr. Fu treats the entire spectrum of shoulder conditions, including rotator cuff tears, shoulder instability, and shoulder arthritis. Dr. Fu was educated at Columbia University and Yale School of Medicine, followed by orthopedic surgery residency at HSS and sports medicine & shoulder surgery fellowship at Rush University Medical Center in Chicago. He has been a team physician for the Chicago Bulls, Chicago White Sox, DePaul University, and NYC’s PSAL.
Disclaimer: All materials presented on this website are the opinions of Dr. Michael Fu and any guest writers, and should not be construed as medical advice. Each patient’s specific condition is different, and a comprehensive medical assessment requires a full medical history, physical exam, and review of diagnostic imaging. If you would like to seek the opinion of Dr. Michael Fu for your specific case, we recommend contacting our office to make an appointment.